National Women’s Health Week is May 12 to 18. Each year at this time, millions of women are reminded to take steps to make their health—including mental health and emotional well-being—a priority. In honor of Women’s Health Week, this blog focuses on postpartum mood disorders, one of the most common mental health issues women struggle with.
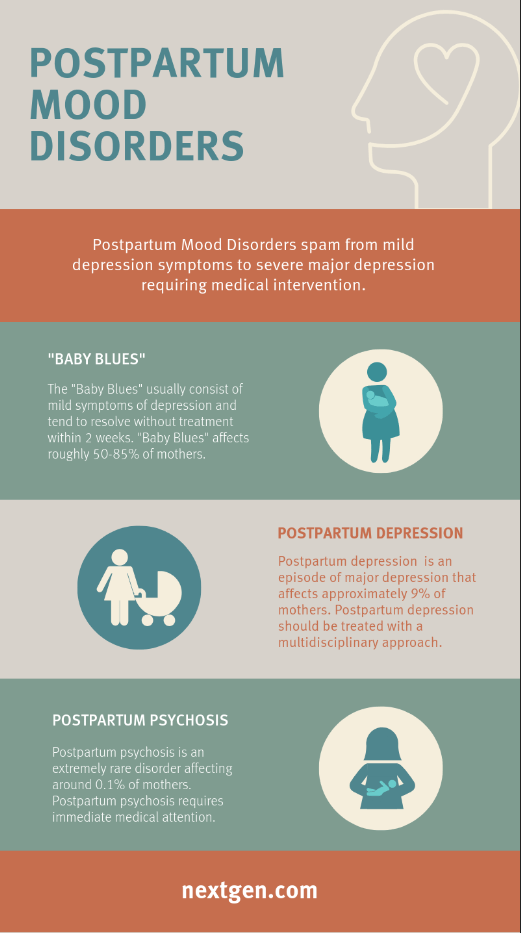
Postpartum mood disorders span a spectrum: from mild symptoms of depression, often described as “baby blues,” which usually resolve without treatment in about 2 weeks, through severe major depression, which requires intensive medical interventions. Baby blues develops in roughly 50% to 85% of women and is thought to be related to the rapid hormonal changes experienced after delivery. Postpartum depression, on the other hand, is an episode of major depression that affects about 9% of mothers a year.
It is not clear what exactly causes postpartum depression; factors that may be involved include genetic susceptibility and hormonal changes following delivery, as well as the presence of psychological and social problems such as marital problems, financial difficulties or housing insecurity. Interestingly, two important risk factors for developing postpartum depression are its prior occurrence with a previous pregnancy or having experienced depression any other time unrelated to pregnancy.
Postpartum depression not only causes anguish and suffering for the mother, it has also been shown to result in less favorable infant outcomes. The depression often interferes with breastfeeding, maternal and infant bonding and the wellbeing of other children in the family and may negatively impact the mother’s relationship with her partner.
It is extremely important to recognize postpartum depression. Unrecognized and untreated postpartum depression takes a heavy toll; recognized, it is an extremely treatable disorder. In this context, there are clear guidelines for screening all women after delivery for symptoms of depression. Multiple screening tools are available for this purpose, including several specific to postpartum depression and those used to screen for depression in other clinical settings like the commonly used Patient Health Questionnaire-9 (PHQ-9). It can be equally important to ask questions during a clinical encounter about mood, mood swings, sadness, irritability and emotional lability. This can be a good way to reassure women that what they are experiencing is “normal” and felt by many other women after delivery (such as postpartum blues), and if symptoms point toward postpartum depression, a physician can immediately put a treatment plan in place, including close follow-ups.
Caring for patients with postpartum depression requires a multidisciplinary approach and might involve a psychiatrist, obstetrician, pediatrician (caring for the newborn), the mother’s family physician and other care team members. The healthcare information technology (HIT) environment that supports and enables this integrated care must allow real-time flow of clinical information at times across multiple organizations and, certainly, several disciplines. The NextGen® Share interoperability platform provides real-time access to 230 million patient records across 4 billion encounters with Carequality and Surescripts. It is this flow of information that allows early detection and early treatment of women with severe postpartum depression.