Practices have a lot on their plates when it comes to medical billing. Effective practice management can boost efficiency, enhance patient convenience, and optimize revenue. However, when errors occur anywhere in the revenue cycle, you increase your administrative workload—and may even lose revenue.
The revenue cycle journey affects every aspect of your practice, including patient satisfaction, provider experience, and financial and clinical outcomes. In this upcoming blog series, we will explore all areas of this journey. Our goal is to help your practice minimize lost revenue and reduce administrative overload due to errors occurring in the revenue cycle. The first step is understanding the links in your revenue chain.
Timing is everything
When it comes to medical billing and claims follow up, timeliness and accuracy are essential. Most states require health insurers to pay claims within 30 or 45 days. Specific time frames vary depending on the insurance payer.
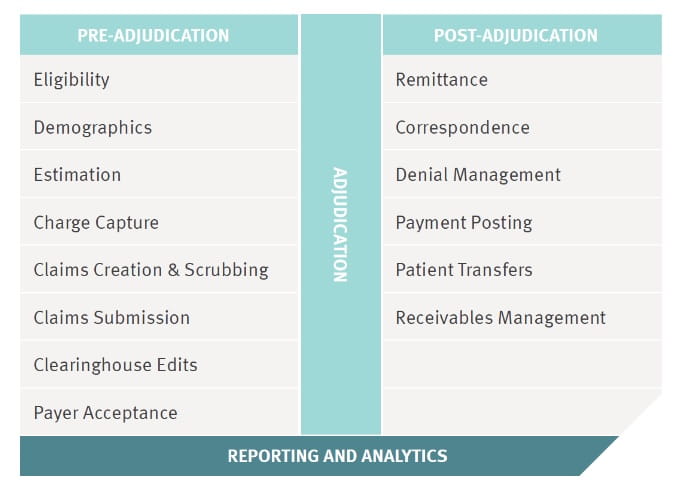
After filing a claim, several things must happen before a medical practice receives a payment or is informed of a denial. Understanding this chain of events will help you identify broken links. It can help you resolve issues that may lead to denials.
Every stage of the revenue cycle must be managed to ensure doctors are fairly compensated, and patients who received services get their allowed insurance coverage.
In our next blog in the series, we will explore patient eligibility and demographics, as well as how to collect patient information during the visit.
To learn more, read A Simple Guide: Practice Management and Medical Billing.