As more people become aware of remote patient monitoring (RPM) devices and their benefits, the pressure for your practice to include them will only increase. Your practice can capitalize on this growing interest and insight by beginning to offer devices to help manage chronic conditions, like blood pressure cuffs and glucometers, sooner than later.
RPM encourages people to engage more deeply in their own health, which in turn keeps them in closer contact with you. Chronic care management requires consistent care that can provide insights for treatment and improve health outcomes. An RPM device in the home means more measures and fewer in-person appointments to measure vital signs.
RPM benefits
Health monitoring devices enable physicians to:
- View patients’ data in real time
- Gain more insights to achieve better outcomes
- Obtain vital data without the need for an in-person visit
- Support clinical decisions with data that flows directly into the EHR
- Track chronic conditions more closely
Visit Benefits of Health Monitoring: Extending Care Beyond the Walls of Your Practice to learn more.
This six-step plan offers a clear path for your providers and patients to get started.
Step 1: Determine your goals
Before you capture your patient’s vital measurements in real time, establish your use cases, define your target patient population, and determine your goals.
Top use cases
This depends on the type of practice. Across the NextGen Healthcare client base, use cases include:
- Hypertension
- Diabetes
- Multi-condition (Hypertension and Diabetes)
During this stage, take some time to plan the process of documenting clinical workflows. Start with how you are delivering care now and adjust it to how you want to deliver care beyond the walls of the clinic. Consider evidence-based guides, such as The 7-Step Self-Measured Blood Pressure (SMBP) Quick Guide from the American Medical Association (AMA). You may need to make a few adjustments as you roll out your program.
By establishing measurements for evaluation, you’ll improve the likelihood of reaching milestones that lead to successful clinical and financial outcomes.
Step 2: Integrate RPM into your virtual care and EHR
Once you have your goals and use cases identified, determine the technology you plan to use, create your device provisioning plan, and develop your communication strategy, including RPM consent language.
What are the steps to improve practice efficiency, provide patient and provider convenience, and integrate RPM data into the EHR?
Practices should consider the capabilities of RPM technology to:
• View your remote patient monitoring display from your virtual visit platform—this makes it easy to review patient measures during a virtual visit
• Select and send relevant measures to the EHR to support treatment recommendations
• Send alerts when patient data is outside of a specified threshold or if the patient has missed readings
• Help people understand how to sync their device via Bluetooth with a mobile app so they can set it and forget it
• Enable people to see their goals and readings
Step 3: Meet staffing requirements for RPM
The number of staff involved in the RPM program will be based on your practice’s goals and patient population. If your practice has been awarded a grant, you will need someone to manage the grant’s requirements and expectations.
Step 4: Set up your health IT solutions and support
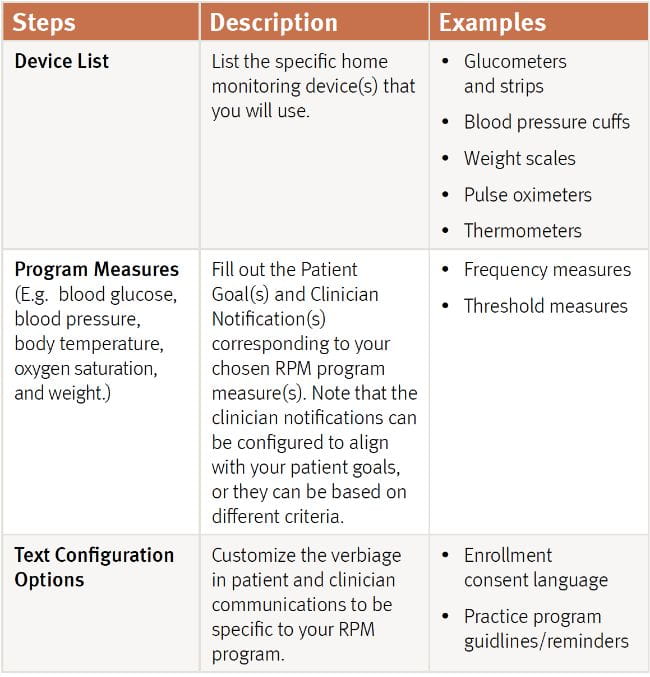
Consider the following for the design of your RPM program technology:
• Library of FDA-approved remote patient monitoring devices—supports connections to devices under multiple therapeutic categories
• An enterprise platform approach to RPM—supports diverse use cases and conditions
• Integrated RPM data and visuals—enables vital information to flow directly into the clinical workflow for virtual care, EHRs, and care management
• Scalability and cost efficiency across broad populations—includes logistics, procurement, and technical support services
Step 5: Decide what's best for your practice: patient-owned or practice-owned device?
Both models have benefits.
Patient-owned devices remain with the patients and may be reimbursed by the patient’s insurance provider. The device will not need to be returned or cleaned, and the patient may continue to use it after they graduate from your RPM program.
Practice-owned devices can be given to patients who cannot receive devices from their payor (not reimbursable) or other free programs. Practices should consider how they prioritize specific patient populations for RPM distribution, track the lending process, and handle post-program returns (cleaning and data removal).
Step 6: Conduct training and education
Design your training with the end-user in mind. Will these care team members enroll patients, review patient data, or support the technology? Consider developing an RPM toolkit for staff and patients. Your toolkit can consist of educational videos, brochures, and frequently asked questions. Visit Remote Patient Monitoring Toolkit to learn more.
How do you get your providers and staff to support patient adoption?
Initiate program kickoff sessions with your care team and then schedule a follow-up session to review progress. This will help ensure your program is successful in meeting the needs of your patients.
Members of your care team can role play as patients and experience the RPM program from the patient’s perspective. If your RPM solution tracks enrollment and measurement activity, you can share the engagement status of your target patient population internally.
Again, a toolkit packed with marketing and educational resources can help get the word out to your patients, particularly those with chronic conditions. In addition to empowering people to have a more active role in their healthcare, your physicians will gain more insight into their health between visits.
For more details on how to launch and manage an RPM program for your practice, read Expand Patient Care with Remote Patient Monitoring (RPM).