As we travel across the country sampling dishes of health industry transformation, it’s clear that national tastes are changing. We've observed a desire for new flavors and concern about waste (and waistlines), along with new regulatory guidelines.
All this opens opportunities for healthcare organizations to serve new offerings. Here’s a recipe for interoperability success.
Ingredients
- 18 different EHR vendors
- Two to three hospital systems
- 1,200 Physicians
- New value-based care payment arrangements
- Engaged patients
Start with 18 different EHR vendors. Put interoperable records in a large mixing bowl.
Eighteen—that’s the number of EHR systems used by the affiliated providers of an average hospital.1 That means 18 EHRs must speak the same language for clinical data exchange to occur.
Interoperable records enable doctors, nurses and other clinicians to see a full picture of their patients’ medical history and make the best possible clinical decisions. Today patients expect care teams to have that full picture, collaborate on care plans, and act upon a fully informed profile when providing care.2
Arrange care sites as endpoints. Garnish with intelligent information exchange.
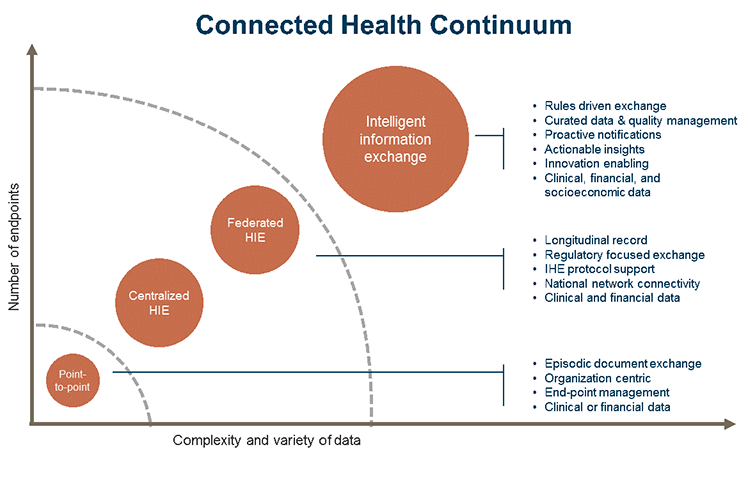
Establishing a continuum of connected health requires organizations to move beyond simple document shipping from point A to point B. Facile document exchange has an important role in getting a network effect started, but long-term success requires organizations to add automation, data quality management, and integrated workflow insights (see Connected health continuum.)
Folding an interoperability strategy into larger population health goals helps to ensure that use-cases align to deliver the most value for your organization and patients.
Cover interoperable records with value-based care payment arrangements. Form into improved outcomes.
As the healthcare industry transitions to a greater percentage of payments from value-based contracts, and care delivery organizations take on direct risk for quality outcomes, those that fail at local and national interoperability will likely miss out on potential benefits. Seventy-four percent of healthcare executives believe that robust interoperability is critical for value-based care.
Today, stakeholders want to leverage their data—and their community’s data—to directly support current health industry initiatives aligned with the quadruple aim. Organizations need to be able to aggregate clinical data, incorporate non-traditional data sources, trigger actionable insights, and support data access for third-party developers.
This year has seen a tipping point towards realizing the goals of data exchange. Providers now have a clear recipe for how to enable successful data exchange within a community and across the country.
To really delight diners, bake interoperability into your workflows. Remove barriers to choosing the cuts they enjoy most.
- Automate where possible. Setup your data exchanges to operate transparently in the background. Use recurring workflows—such as patient check-in, encounter creation, and the signing of a completed chart—as trigger events to push to, pull from, or query external systems that are important to care.
- Support, and then move past, C-CDAs. Today’s primary vehicle for communicating patient-specific clinical data is the C-CDA. Organizations have often found these documents to be excessively burdensome; some partners choose the everything-plus-the-kitchen-sink approach to sharing patient information. Organizations looking to succeed at value-based care need to support C-CDA incorporation, but also target and make it easy to manage specific data exchange elements such as meds, allergies, and care plans through FHIR-based APIs, which are lighter weight and more precise.
- Share—don’t block. Healthcare entities sometimes fail to provide equal access to information. For example, one study found that hospitals are less likely to exchange clinical summaries with hospitals outside their health system that don't share the same EHR vendor.3 Later this year, we expect the ONC to release long-awaited final rule on information blocking.4
- Choose the right vendor. Recent mergers, acquisition, buy-outs, and market pressures have created an unstable future for many healthcare technology vendors, leading to potential disruptions in delivery to organizations that rely on their products and services. The shaky marketplace may also interfere with future upgrades of connectivity solutions and interface engines or the development of new solutions.5
Add national connectivity. Serve as a well composed dish.
Enabling secure provider-to-provider and organization-to-organization connectivity has never been easier. Organizations today can enable Direct messaging and Carequality connectivity to turn on immediate access to nearly any provider or health system.
Direct messaging continues to deliver immediate value for all players in the healthcare continuum. Usage continues to grow. Stakeholders consumed 65.5 million Direct exchange transactions in the third quarter of 2018, an increase of 41% over the same period last year. The cumulative total of Direct exchanges served climbed to nearly 497 million at the end of the third quarter6.
Under the Carequality Interoperability Framework, more than 50% of all health care providers in the country are now empowered to share health data.7 Carequality is designed to be largely invisible to physicians and other individual users; it works in the background of EHR workflows to enable clinical data exchange between disparate EHR and vendor networks. To date, more than 1,400 hospitals, 40,000 clinics, and 600,000 healthcare providers are connected through Carequality.
Look for a great pairing.
Healthcare practices and organizations need a stable technology partner to help them navigate the less-than-perfect world of cross-platform connectivity. This partner should:
- Advise you regarding both clinical and financial aspects of cross-platform connectivity
- Provide professional consultation and support to help you grow practice or organization as well as offering technology support
- Demonstrate a history of stability
NextGen® Connected Health solutions seek to achieve better patient care through connectivity everywhere. Read this guide to find out more. Let's get connected.
[1] Tom Sullivan, "Why EHR Data Interoperability Is Such a Mess in 3 Charts," Healthcare IT News, May 16, 2018, https://www.healthcareitnews.com/news/why-ehr-data-interoperability-such-mess-3-charts.
[2]Michael F. Furukawa, Jennifer King, Vaishali Patel, et al. September 2014. "Despite Substantial Progress in EHR Adoption, Health Information Exchange and Patient Engagement Remain Low in Office Settings," Health Affairs 33 (9). https://www.healthaffairs.org/doi/10.1377/hlthaff.2014.0445.
[3] Anabel F. Castillo, Marvin Sirbu, and Alexander L. Davis, "Vendor of choice and the effectiveness of policies to promote health information exchange," BMC Health Services Research, June 4, 2018, https://bmchealthservres.biomedcentral.com/track/pdf/10.1186/s12913-018-3230-7.
[4] Mandy Roth. "Countdown to Information Blocking Rule In Progress," HealthLeaders, September 28, 2018, https://www.healthleadersmedia.com/innovation/countdown-information-blocking-rule-progress.
[5] Chris Keall, "Diagnosing the Orion Health buyout deal: A Q&A," The New Zealand Herald, October 1, 2018. https://www.nzherald.co.nz/business/news/article.cfm?c_id=3&objectid=12133606.
[6] "DirectTrust Continues Steady Growth in Number of Direct Exchange Users, Addresses and Transactions During Third Quarter," GlobalNewswire, October 24, 2018. https://globenewswire.com/news-release/2018/10/24/1626383/0/en/DirectTrust-Continues-Steady-Growth-in-Number-of-Direct-Exchange-Users-Addresses-and-Transactions-During-Third-Quarter.html
[7] "Carequality Trusted Exchange Framework Facilitates Exchange of Nearly 60 Million Clinical Documents in First Two Years," GlobalNewswire, October 24, 2018. https://globenewswire.com/news-release/2018/10/24/1626272/0/en/Carequality-Trusted-Exchange-Framework-Facilitates-Exchange-Of-Nearly-60-Million-Clinical-Documents-in-First-Two-Years.html